Welcome to WellSpace Health
The mission of WellSpace Health is achieving regional health through high quality comprehensive care: It's about achieving health, not just …
Read More WellSpace Health’s Behavioral Health programs have served the Sacramento region since 1953. We have over 60 years of experience identifying service gaps and filling them, care transition gaps and bridging them, and we are always in the process of building programs to meet emerging needs. As a result, our robust Health Center network has Behavioral Health programs built into our primary care delivery, but we can also ‘wrap’ the people we serve in a host of ancillary programs so that we can address the whole person and the whole family. To maximize the ease of access for our clients, our behavioral health services can be accessed separately or alongside / integrated in to our health services.
WellSpace Health’s Behavioral Health programs have served the Sacramento region since 1953. We have over 60 years of experience identifying service gaps and filling them, care transition gaps and bridging them, and we are always in the process of building programs to meet emerging needs. As a result, our robust Health Center network has Behavioral Health programs built into our primary care delivery, but we can also ‘wrap’ the people we serve in a host of ancillary programs so that we can address the whole person and the whole family. To maximize the ease of access for our clients, our behavioral health services can be accessed separately or alongside / integrated in to our health services.
Our Health Access, Referral & Treatment (HART) care transition services are designed to address the “additional vital signs” our clients have. For example, by declaring “homelessness as a vital sign,” Wellspace Health is asserting the fact that those persons we serve who have no home also have exacerbated health and behavioral health conditions, and these conditions become less acute and more amendable to change and treatment when homelessness is addressed. Similarly, a person whose psychiatric care is being provided in a separate location from primary care and funded by a completely different funding stream may benefit from case management to ensure integrated care. Following are WellSpace Health’s key HART programs.
This nationally recognized program was developed to triage persons who are high utilizers of non-urgent care in area emergency departments to ensure that they do not have urgent health care needs, transport them to an appropriate health center location, and treat them in a place where they can establish routine health care. This “whatever-it-takes” program also provides assertive case management to ensure that other vital signs (income, medical home, independent living skills, homelessness, etc.) are addressed. The program brings people to the right treatment in the right place at the right time and establishes their ongoing health care so that treatment can shift from a reactive to proactive perspective and free up urgent and acute care settings for higher acuity patients. Every $1 spent on this program returns a savings of $10 in emergency department costs.
This program was developed to assess the care navigation needs of any patients in emergency departments. Information, referral, brief motivation, and support in care transition are provided. Intakes for eligible patients are completed inside Emergency Departments for T3 Case Management services.
This program was developed to assess the care navigation needs of patients who are currently admitted. This program compliments the hospital-based social work departments that are typically focused on the inpatient experience, established care connections and transition plans for patients early in the hospital stay. Upon discharge, Case Management services continue to help reduce hospital readmission.
Rather than keep a homeless person in an inpatient setting for long periods of time to ensure appropriate medical needs are met and to prevent readmission, this nationally recognized program coordinates the placement of persons who are homeless and needing additional respite care in a nurse-managed specialized unit maintained and operated by WellSpace Health within the Salvation Army and other area shelters. Clients are offered 3 meals a day, modified rules, bed rest, nurse care and self-care. Case Managers provide transportation to ongoing health and other treatment services, assisting with housing placement, and other assertive community treatment supports. The program supports safety, independence and autonomy for persons served and reduces their hospital stays by an average of 23 days.
Our Co-Occurring Continuum provides treatment for substance use disorders and mental health disorders in a variety of settings designed to meet the unique needs of each patient. The licensed and certified staff of the Co-Occurring Continuum utilize evidence-based curricula and the resources available through WellSpace Health to deliver compassionate, whole-person care in Joint Commission Accredited environments.
Our facility located in North Sacramento offers both withdrawal management (detox) and residential treatment for substance use disorders and co-occurring mental health disorders. The facility is staffed 24 hours a day. Withdrawal Management patients are medically cleared prior to entry, and may receive prescriptions for a brief time while they adjust. The Residential Treatment program has on-site master’s level therapists in addition to registered and certified substance abuse counselors, and offers 31 hours of programming a week. Both programs are co-ed. The patient may arrange for private payment, otherwise they must be cleared and referred by the Sacramento County System of Care (916) 874-9754.
Outpatient treatment for substance abuse is available at our J Street facility. Our staff provide individual assessments, and work collaboratively with patients to design a treatment plan that meets their needs. Urine drug testing is provided, and groups are offered at various times in order to accommodate most schedules. Most patients qualify for their payments to be made through Drug Medi-Cal. Patients may call (916) 313-8434 for more information.
This program, also located at our J Street facility, provides medication to assist in recovery from opiate and alcohol use disorders. Patients are screened by our counseling staff and are co-enrolled in our outpatient program. Patients who meet the criteria can be offered Vivitrol or Buprenorphine, prescribed and monitored by qualified medical providers. Patients may call (916) 313-8434 for more information.
In addition to the publicly available services above, WellSpace Health provides counseling, drug testing, and case management services to Sacramento County in the Adult Drug Court and in the Rio Cosumnes Correctional Center. We also provide substance use disorder counseling and mental health medication management services to Saint John’s Program for Real Change.
Welcome to WellSpace Health’s Behavioral Health Program! We currently offer Integrated Behavioral Health (IBH) services to our adult patient population at five of our Federally Qualified Health Centers (FQHCs) in the greater Sacramento area. The services are an integrated part of primary care and the program is a collaborative care approach to treating patients based on the IMPACT model pioneered by Dr. Jürgen Unützer at the AIMS Center of the University of Washington. IBH services include psycho-education, counseling, and medication management for patients with behavioral issues such as depression, anxiety, trauma, or adjustment to psychosocial stressors, as well as consultation services for providers, and case management services for patients.
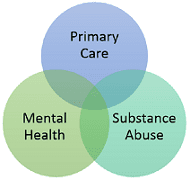
Integrated Behavioral Health services are for existing primary care patients of WellSpace Health regardless of income or insurance. Patients who are uninsured may qualify for a sliding fee. Currently we are only serving adults but we plan to expand to children in the near future. The referral for IBH services must come from the WellSpace Health Primary Care Provider (PCP), however, patients may request the services from any staff and they will be guided appropriately to access the services. Patients are systematically screened with the Patient Health Questionnaire (PHQ-9) to identify symptoms and assess for risk. Patients who qualify for services include patients who are adjusting to a newly diagnosed medical condition, struggling to effectively manage a chronic condition (i.e., diabetes, cardiovascular disease, and chronic pain), suffering from insomnia, depression or anxiety, working on lifestyle changes (i.e., smoking cessation, weight management) or referred by their PCP for other issues. By providing services at multiple locations, we are able to increase patient access to services and ensure continuity of care.
In the IBH model, the Primary Care Provider (PCP) is still the provider who is in charge of the patient’s care. Additionally, the PCP will continue to prescribe antidepressants as needed. But with the addition of IBH services, whenever a patient with behavioral health needs is identified, a member of the IBH team will be available during clinic hours to attend immediately to that patient’s needs.
IBH Clinicians, who hold a license in Social Work or Psychology, are responsible for the initial and follow-up Integrated Behavioral Health assessments, short-term counseling, psycho-education around behavioral health symptoms, supporting medication management by PCPs, and providing psycho-educational groups.
IBH Care Coordinators are the support staff responsible for facilitating patient engagement in program, contacting patients between visits to track progress and motivating patients to continue treatment, conducting behavioral activation services over the phone with patients who have challenges accessing on-site services, and facilitating patient referrals to other mental health services and community resources.
A Psychiatry Care Advisor, who is a psychiatrist is available by phone during clinic hours to consult with the PCPs, present in-services at regularly scheduled provider meetings, and consult with clinicians on complex cases during weekly caseload reviews and as needed by phone.
Psychiatry providers, who are either a psychiatrist or psychiatric nurse practitioner, are available to primary care patients who need medication management at a level of care that is higher than the scope of the PCP. Patients who receive medication management from a psychiatry provider may or may not also be engaged in short-term counseling with an IBH Clinician.
Share this page with a friend:
The mission of WellSpace Health is achieving regional health through high quality comprehensive care: It's about achieving health, not just …
Read MoreConnecting You to Care WellSpace Health is committed to serving all patients/clients, regardless of their ability to pay. Although we do …
Read More